JOURNAL OF ORTHOPAEDICS AND CLINICAL RESEARCH
Femoro-popliteal Artery Bypass and Transmetatarsal Amputation Followed by Delayed Forefoot Flap
Michael Mayombo I1,2,3*, Othmane Belmaachi1 and Youssef Ettaoumi1
1Cardiovascular Surgery Department, University Hospital Center of Casablanca, Morocco
2Marthenica Private Clinic, Gabon
3Koma and Landji Private Clinic, Gabon
*Corresponding Author: Michael Mayombo Idiata, Cardiovascular Surgery Department, University Hospital Center of Casablanca, Morocco, Marthenica Private Clinic, and Koma and Landji Private Clinic, Gabon.
| ReceivedFeb 2, 2024 | RevisedFeb 27, 2024 | AcceptedMar 6, 2024 | PublishedMar 20, 2024 |
Abstract
Critical limb ischemia (CLI) is a severe blockage in the arteries of the lower extremities, which markedly reduces blood-flow. It is a serious form of peripheral arterial disease, or PAD, but less common than claudication. PAD is caused by atherosclerosis, the hardening and narrowing of the arteries over time due to the buildup of fatty deposits called plaque.
CLI is a chronic condition that results in severe pain in the feet or toes, even while resting. Complications of poor circulation can include sores and wounds that won't heal in the legs and feet. Left untreated, the complications of CLI will result in amputation of the affected limb.
The authors present a patient with CLI, and a left forefoot gangrene treated with multi-stage operations (femoro-popliteal arterial bypass, transmetatarsal amputation and delayed forefoot free-flap) with good results.
Keywords
Critical ischemia; Bypass; Transmetatarsal amputation; Flap
Introduction
According to the PAD guidelines by the European Society for Cardiology [1,2], CLI was replaced by the new concept of chronic limb threatening ischemia (CLTI) though it is not yet a common term in the vascular surgery field. Critical limb ischemia (CLI) is a severe blockage in the arteries of the lower extremities, which markedly reduces blood-flow. It is a serious form of peripheral arterial disease, or PAD, but less common than claudication. PAD is caused by atherosclerosis, the hardening and narrowing of the arteries over time due to the buildup of fatty deposits called plaque. CLI is a chronic condition that results in severe pain in the feet or toes, even while resting. Complications of poor circulation can include sores and wounds that won't heal in the legs and feet. Left untreated, the complications of CLI will result in amputation of the affected limb. Critical Limb Ischaemia is the advanced form of chronic limb ischaemia.
It can be clinically defined in three ways:
• Ischaemic rest pain for greater than 2 weeks duration, requiring opiate analgesia
• Presence of ischaemic lesions or gangrene objectively attributable to the arterial occlusive disease
• ABPI less than 0.5
On examination, the limbs may be pale and cold, with weak or absent pulses. Other signs include limb hair loss, skin changes (atrophic skin, ulceration, or gangrene), and thickened nails [3].
Critical limb ischemia occurs over several weeks to months but is at the extreme end of the spectrum of chronic limb ischemia (Rutherford classification 4-6, Fontaine III/IV-Table 1).
|
Symptom complex |
Rutherford classification |
Fontaine classification |
|
|
Asymptomic |
Stage 0 |
Stage I |
|
|
Intermittent claudication |
Mild claudication |
Stage 1 |
Stage IIA (Symptoms with>200 meters walking) |
|
Moderate claudication |
Stage 2 |
Stage IIB (Symptoms with>200 meters walking) |
|
|
Severe claudication |
Stage 3 |
||
|
Critical limb ischemia |
Rest pain |
Stage 4 |
Stage III |
|
Ischemic ulceration(limited to digits) |
Stage 5 |
Stage IV |
|
|
Severe ischemic ulceration or frank gangrene |
Stage 6 |
Table 1: Rutherford and fontaine classifications of chronic peripheral arterial disease severity [4].
The authors report a patient who underwent multi-stage operations for the treatment of CLI (femoro-popliteal arterial bypass, transmetatarsal amputation and delayed forefoot free-flap) with good results.
Case Report
A 65-year old male patient was admitted to the facility with left forefoot gangrene. The patient experienced resting pain for several months. His risk factors were age, smoking, diabetes, high cholesterol and tobacco use. The diagnosis was Rutherford class 6 CLI.
The ABI was unreliable as its diagnostic sensitivity among diabetic patients is slow. CT angiography was consistent of left superficial femoral artery and anterior tibial artery thombosis.

Figure 1: Gangrene of the left forefoot on admission.
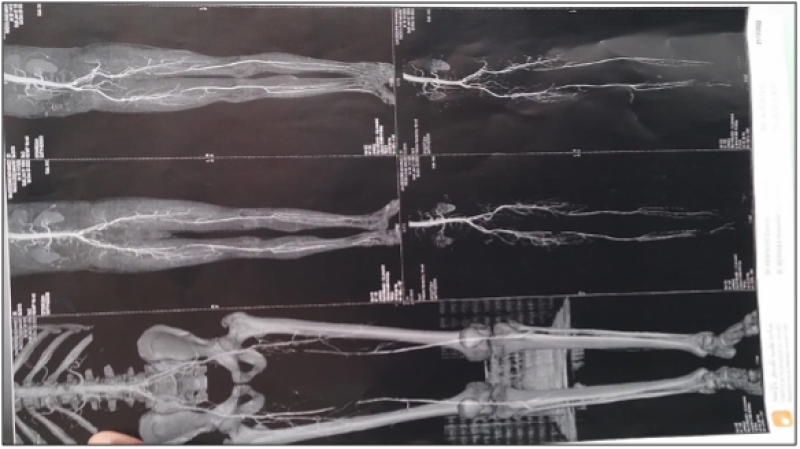
Figure 2: CT-angiography of the aorta and the lower limbs arteries.
On arrival, the patient was treated with antibiotics, anticoagulants and pain killers.
Then, the wound was debrided under anesthesia and the treatment options were explained. At that time, the doctors could not do a single-stage operation with vascular and plastic surgery teams. Firstly, the authors did a femoro-popliteal bypass and a transmetatarsal amputation (Figure 3 and 4).
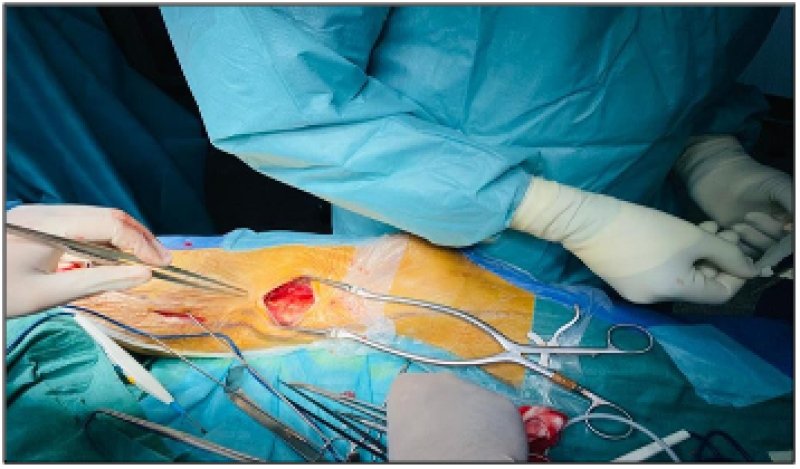

Figures 3 (a,b): Left femoropopliteal bypass via the reversed internal saphenous vein.
The surgery was under rachianesthesia. The doctors first performed the bypass to repermeabilize the anterior tibial artery. Then the doctors performed the transmetatarsal amputation. The patient received heparin during surgery. The surgery duration was 3 hours.

Figure 4: Left transmetatarsal amputation.
The immediate post-operative period was unremarkable. The patient was discharged on POD #4 with a prescription, a dressing change at a medical center nearby his house with a close follow-up with the team. A reconstructive surgery was scheduled with the plastic surgery team.
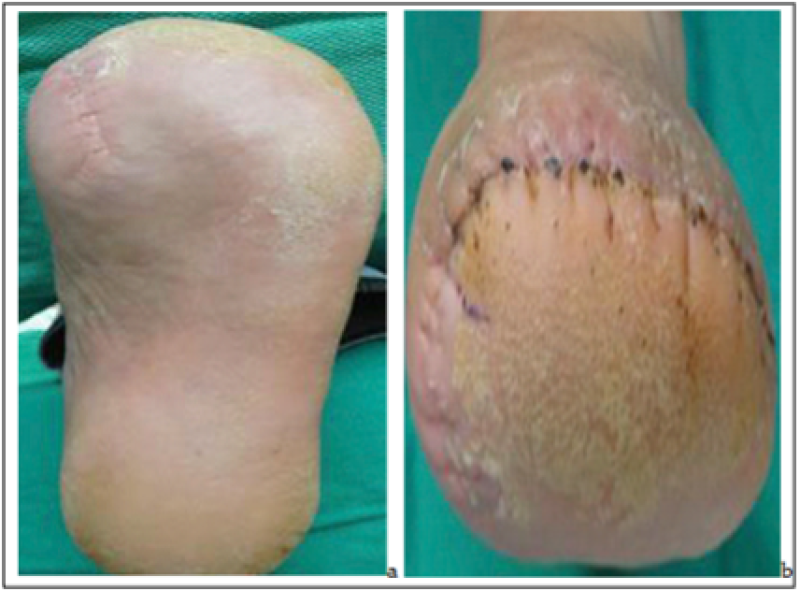
Figure 5(a,b): Delayed forefoot flap after transmetatarsal amputation.
Discussion
The debate constitutes regarding whether to treat these patients using multi-stage operations or as a single-stage operation. Some authors recommend performing the bypass or endovascular treatment first followed by free flap coverage as the doctors did [5,6]. However, though the published literature is limited regarding the single-stage treatment, simultaneous arterial bypass and free flap is feasible [7,8].
The doctors chose to perform multi-stage operations (femoro-popliteal arterial bypass, transmetatarsal amputation and delayed forefoot free-flap) with good results. The follow-up period is only one year instead of Fodor MM, et al. [8], with a follow-up period of 13 years.
Permeability of the femoro-popliteal artery bypass and the microvascular anastomosis to the anterior tibial artery were confirmed by computed tomography angiography (CTA) performed 13 years postoperatively. There is a range of therapeutic options for treating foot lesions depending on the causes and mechanisms of development. It is clear that several different departments must collaborate to perform treatment on such patients. The treatment should involve not only physicians but medical staff, because there are many aspects of treatment which can be covered only by medical staff. Multidisciplinary treatment is therefore a key word for CLI treatment [9]. But in this setting, the collaboration with peripheral health centers and university hospitals is not strong as recommended. So, the authors are constructing a new collaboration system based on this approach in the regional network.
Conclusion
Multidisciplinary treatment is the key in the treatment of CLI. Depending on the setting, a single-stage or multi-stage vascular and plastic surgery reconstruction (arterial bypass and free flap) are feasible methods for lower limb salvage in those patients. Therefore, prevention not to develop CLI is more important than to treat aggressively after progression to such a severe state.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from anyone.
References
1. https://health.ucdavis.edu
2. Aboyans V, Ricco JB, Bartelink ML, Björck M, Brodmann M, Cohner T, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in Collaboration with the European Society for Vascular Surgery (ESVS). Kardiol Pol. 2017;75(11):1065-160. PubMed | CrossRef
3. https://teachmesurgery.com
4. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG. Inter-society Consensus for the Management of Peripheral Arterial Disease. Int Angiol. 2007;26(2):81-157. PubMed | CrossRef
5. Briggs SE, Banis Jr JC, Kaebnick H, Silverberg B, Acland RD. Distal Revascularization and Microvascular Free Tissue Transfer: An Alternative to Amputation in Ischemic Lesions of the Lower Extremity. J Vasc Surg. 1985;2(6):806-11. PubMed | CrossRef
6. Meyer A, Goller K, Horch RE, Beier JP, Taeger CD, Arkudas A, et al. Results of Combined Vascular Reconstruction and Free Flap Transfer for Limb Salvage in Patients with Critical Limb Ischemia. J Vasc Surg. 2015;61(5):1239-48. PubMed | CrossRef
7. Igari K, Kudo T, Toyofuku T, Jibiki M, Inoue Y, Tanaka K, et al. Combined Arterial Reconstruction and Free Tissue Transfer for Patients with Critical Limb Ischemia. Ann Vasc Dis. 2013;6(4):706-10. PubMed | CrossRef
8. Fodor MM, Fodor L. Simultaneous Femoro-popliteal Artery Bypass and Foot Free Flap for Lower Limb Salvage: A 13-year Follow-up. J Int Med Res. 2021;49(5):3000605211012607. PubMed | CrossRef
9. Komai H. Multidisciplinary Treatment for Critical Limb Ischemia in Peripheral Arterial Disease. Ann Vasc Dis. 2019;12(2):151-6. PubMed | CrossRef
Michael Mayombo I1,2,3*, Othmane Belmaachi1 and Youssef Ettaoumi1
1Cardiovascular Surgery Department, University Hospital Center of Casablanca, Morocco
2Marthenica Private Clinic, Gabon
3Koma and Landji Private Clinic, Gabon
*Corresponding Author: Michael Mayombo Idiata, Cardiovascular Surgery Department, University Hospital Center of Casablanca, Morocco, Marthenica Private Clinic, and Koma and Landji Private Clinic, Gabon.
Copyright© 2024 by Mayombo M, et al. All rights reserved. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Mayombo M, Belmaachi O, Ettaoumi Y. Femoro-popliteal Artery Bypass and Transmetatarsal Amputation Followed by Delayed Forefoot Flap. J Orth Clin Res. 2024;2(1):142-47. DOI: https://doi.org/10.37191/Mapsci-JOCR-2(1)-015
